I recently had a follow up appointment with a patient of mine. “Sam” came to our clinic after having failed attempts of treatment from standard Physical Therapy and chiropractic care. His past physical therapist had given him generalized stretching with little to no benefit, and by the time I evaluated him, Sam admitted that, “(he) was not impressed with his therapy treatment.” He had heard about Nick Rinard Physical Therapy, and he was hoping to get the results he desired with us.
During his initial evaluation, Sam presented with limited, painful movements in several motions of the shoulder. The most painful motion was the motion of putting the arm behind him (like he was going to scratch in between his shoulder blades). Incidentally, this was also the motion which initially caused his pain three months ago.
 I had Sam passively stretch into the painful motion. This was not a random decision. It was a clinical decision based off of his baselines and has been clearly documented and researched by the works of Mark Laslett. As Sam repeated this movement, the pain dissipated and all of his baselines improved. Sam continued to perform this exercise until his next visit, at which, he reported 95% improvement.
I had Sam passively stretch into the painful motion. This was not a random decision. It was a clinical decision based off of his baselines and has been clearly documented and researched by the works of Mark Laslett. As Sam repeated this movement, the pain dissipated and all of his baselines improved. Sam continued to perform this exercise until his next visit, at which, he reported 95% improvement.
Sometimes the exercise required to fix the mechanical problem is counterintuitive (moving into the pain). A trained mechanical therapist is able to recognize these pain patterns and can make a clinical decision as to what exercise should be performed and interpret the results.
More
By Megan Plante, DPT
21 Mar, 2014
Clinical Case of the Week
BPPV, easily treated, improvement, MDT, Mechanical Diagnosis and Therapies, Mechanical disorder, Nick Rinard physical therapy, Physical Therapy, Portland Oregon, Positive response, vertigo
The most common cause of vertigo (dizziness) is benign paroxysmal positional vertigo (BPPV) and it is a mechanical disorder. A trained clinician can evaluate and treat this condition based off of the patient’s symptoms. The evaluation consists of moving the head into specific positions. Symptoms of BPPV include vertigo with change in head position, nausea with or without vomiting and disequilibrium (poor balance).
Curable
Vestibular System
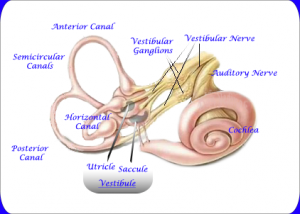
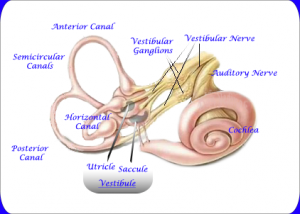
BPPV is a curable condition affecting the vestibular system (inner ear). Your inner ear is comprised of 3 semicircular canals (SCC) and 2 otolith organs. These structures detect head movements (acceleration). Crystals called otoconia are embedded in the otolith organs. Sometimes, the crystals can become dislodged and misplace into the semicircular canals. The misplaced crystals result in increased sensitivity to head movements.
Hopes for a Positive Response
I was treating a patient for low back pain when she mentioned that she was experiencing severe episodes of dizziness. I informed her about BPPV and mentioned that the treatment was very simple and effective. She agreed to have an evaluation in hopes for a positive response.
My patient tested positive for BPPV utilizing the Hallpike-Dix test for the left semicircular canals. I also performed a few other tests and exercises to rule out other potential causes for symptoms. Once we had our diagnosis of BPPV, the treatment was very simple.
Improvement in just one week
I took my patient through a series of head movements that reposition the crystals back into the otolith organs (the saccule and ultricule). After performing the repositioning maneuver, baseline symptoms were decreased and she returned the next week without having any severe episodes of vertigo.
BPPV – A Common Vertigo that is Easily Treated
BPPV is the most common cause for vertigo. Luckily, it is very easy to diagnose and treat with a trained therapist. If you or someone you know has vertigo as a result from head movements, have a physical therapist evaluation so that you may start feeling better today!
More
BACKGROUND:
Up to 80% of the population will experience low back pain (LBP) at some point in their adult life (Croft et al 1997). It is estimated that health care costs for low back pain are larger than for any other disease for which economic analysis is available (Maniadakis and Gray 2000) ($31 billion/year). There is little to no evidence supporting the use of traction, thermal modalities, or electrical stimulation for the treatment of LBP. Unfortunately, these strategies are commonly used for the bulk of LBP treatment. Many studies conclude that the McKenzie method of evaluation and treatment for LBP is superior to that of standard treatment (general stretching and strengthening). What makes the McKenzie approach different is its classification system. Based off of symptom response to repeated lumbar spine movements, patients are classified into 1 of 3 syndromes (derangement, dysfunction, postural). After patients have been classified, their individualized treatment plan is created. The McKenzie method also emphasizes self-treatment and long term symptom management. I consider this the most valued aspect of treatment, as statistics show LBP is recurring in nature. Let’s review a case of a patient with a very successful outcome utilizing the McKenzie method.
SYMPTOMS:
Patient presented to therapy 2 weeks after the onset of LBP with bilateral leg pain. Patient described sharp pain which radiated down to the left foot and down to the right shin. Symptoms started after a weekend of working (auto mechanic) which involved repetitive bending and lifting of heavy equipment. Patient rated worst pain as an 11/10 for the back and a 10/10 for the left leg, occurring on a daily basis. Patient was severely limited with walking, sitting and sleep.
THERAPIST’S EVALUATION AND FINDINGS:
Patient demonstrated pain with all lumbar spine motions in standing. There was no neurological (strength, sensory, reflex, neural tension) deficit. This is important to test when there is a presence of leg pain.
Baseline symptoms= LBP + left foot tingling. Patient was asked to bend forward 10 times, touching his toes. This resulted in increased low back pain, no effect on foot tingling. Bending backwards 10 times also increased LBP with no effect on foot tingling. Patient was then asked to lie on his stomach and perform prone press ups (a back bend using arms to push up into extension). This exercise abolished left foot symptoms, better leaving the clinic that day.
PATIENT HOMEWORK AND OUTCOMES:
Patient was given prone press-ups to be done every hour until his follow up appointment. The next day, the patient returned to the clinic happily reporting that he had not experienced leg pain in over 24 hours! The patient was even able to perform tasks associated with moving into his new home that weekend. In 2 weeks his back pain rating had decreased to a 3/10 and he was experiencing little to no leg symptoms! Patient continued therapy over the next few months with exercise progressions and modifications as needed. At discharge, patient was able to perform his duties as an auto mechanic and continue his training as a member of the National Guard.
HAVE A MECHANICAL EVALUATION FOR YOUR LOW BACK PAIN:
Do not fall victim to chronic low back pain. This is associated with huge healthcare costs, over utilization of medication and surgery. All of which would otherwise be avoided with a simple exercise, requiring no special equipment. The patient from this week’s case left the clinic feeling very empowered by his own ability to treat his symptoms and was no longer considering having major spine surgery.
More
 Lateral epicondylitis, more commonly known as “tennis elbow,” is a pathology that is familiar to physical therapists and the general public. What is lesser known is “pseudo tennis elbow,” a mechanical problem with a very simple solution! Unfortunately, therapists whom are not familiar with the utilization of mechanical diagnosis may unknowingly miss this common elbow derangement. As a therapist practicing the McKenzie method of mechanical diagnosis, I have diagnosed BOTH of my current elbow pain patients as derangements (or pseudo tennis elbow).
Lateral epicondylitis, more commonly known as “tennis elbow,” is a pathology that is familiar to physical therapists and the general public. What is lesser known is “pseudo tennis elbow,” a mechanical problem with a very simple solution! Unfortunately, therapists whom are not familiar with the utilization of mechanical diagnosis may unknowingly miss this common elbow derangement. As a therapist practicing the McKenzie method of mechanical diagnosis, I have diagnosed BOTH of my current elbow pain patients as derangements (or pseudo tennis elbow).
Symptoms
Our patient, “Jane” presented to therapy with intermittent right elbow pain, worsening over the last 3 months. Jane reported difficulty with gripping, lifting, carrying and global limited function of the right arm. Jane described symptoms as “variable” meaning she could perform a task that produced his elbow pain. Then, perform the same task or movement again without experiencing any pain at all! This variability of pain is the hallmark of a derangement and should not be misdiagnosed as a tendonitis, which would indicate inflammation (in which case pain would be constant). Jane rated worst elbow pain as a 6/10.
Physical Therapist Evaluation & Findings
Objective findings included pain with passive elbow flexion and extension as well as pain with active wrist extension and with gripping a tennis ball. Because of my experience as a mechanical therapist, I am familiar with a technique called a mobilization with movement (MWM), developed by Brian Mulligan (a colleague of Robin McKenzie). The mobilization provides a lateral force over the ulna at the elbow joint. While the patient applied this force, she was able to grip the tennis ball PAIN FREE! This same technique was applied for other painful baselines and achieved the same results of ABOLITION OF ALL PAIN! This ability to turn symptoms off with a mobilization indicates an elbow derangement and the MWM is used as the treatment strategy.
Patient Homework and Outcomes
Jane was asked to perform the MWM utilizing the lateral glide while gripping a tennis ball to be performed 10-20 times every hour. The theory is that this mobilization is repositioning the joint in order for it to articulate correctly, resulting in improved range of motion and strength after. Jane returned to the clinic the next day with reports of at least 25% improvement! Objective findings were retested and nearly all baselines had improved in less than 24 hours! Jane returned 1 week later and reported an 85% overall improvement with symptoms.
Get Your Own Mechanical Assessment
Don’t be misdiagnosed! Straightforward pathologies which require one exercise to treat are commonly missed with standard treatment. This results in extra therapy visits, and more of your time and money. It is worth your time to see if your pain has a MECHANICAL component. A simple solution may otherwise be missed.
More
 I had Sam passively stretch into the painful motion. This was not a random decision. It was a clinical decision based off of his baselines and has been clearly documented and researched by the works of Mark Laslett. As Sam repeated this movement, the pain dissipated and all of his baselines improved. Sam continued to perform this exercise until his next visit, at which, he reported 95% improvement.
I had Sam passively stretch into the painful motion. This was not a random decision. It was a clinical decision based off of his baselines and has been clearly documented and researched by the works of Mark Laslett. As Sam repeated this movement, the pain dissipated and all of his baselines improved. Sam continued to perform this exercise until his next visit, at which, he reported 95% improvement.