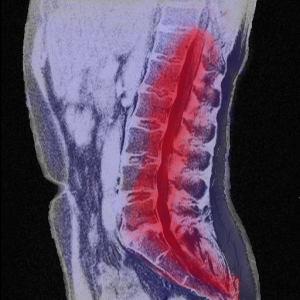
Did you know that 80% of American will experience low back pain in their lifetimes? Take a look at these eye-opening statistics: https://www.thegoodbody.com/back-pain-statistics/
Nick Rinard Physical Therapy uses cutting-edge, scientifically-validated mechanical diagnosis and treatment techniques to help you find the cause and cure of your back pain. Let us help you today.
.
More
Dealing with pain on a daily basis is fatiguing and frustrating. At Nick Rinard Physical Therapy, we empower our patients with individual, customized home exercise programs to help you gain control of your symptoms. We believe in education, and prioritize teaching our patients how to become effective in their daily routines. If you are tired of being a victim to your out of control symptoms, contact us! Our team is dedicated to helping you chart a course to better health.

More
‘Tis the season for making resolutions, focusing on self-improvement, and charting the course for the year ahead. What are you doing to improve yourself in 2018? One small step that can make a tremendous impact in many areas of your life is simply to establish good self-accountability. How credible are you? Many of us are loyal to commitments we make to our friends, family, and coworkers but we may routinely neglect to fulfill our promises to ourselves. When was the last time you put off a work out, failed to follow through with a diet goal, or simply lost momentum with a good training program?
Creating the discipline of good habits is beneficial to all of us! Whether you are looking to reboot your home exercise routine or seeking to redeem your diet after an avalanche of holiday feasts – consistency is the key. Daily diligence defines the difference between crashing through a fad and building a foundation of good habits that can improve your life. In some areas of life, this need for consistency is obvious, for example: brushing your teeth. If you wish to have fresh breath for your date on Friday night, is brushing your teeth just once on Tuesday going to cut it? Nope! Good oral hygiene requires that twice a day commitment every day of the week. Other areas of our health will benefit from applying this daily discipline as well.
So, here are 5 easy ways to help build credibility with yourself and to insure you follow through with all of those good intensions.
- Make an appointment with yourself – Schedule time on your calendar each day, even if it is just 20 minutes, to do your home exercise program. Honor this time the same way you would honor any other medical appointment.
- Reward yourself when you follow through – Improving your health is its own reward, but you may need other tangible incentives to keep you motivated on your course. Make a barter system with yourself – “For every 10 minutes I spend on this treadmill, I will get 10 minutes of guilt-free Netflix ve
- Get friends and family onboard – One of my patients found the best way to correct his posture was to recruit his children, “It’s open season, kids – anytime you can catch me slouching, call me on it and I will give you a dollar.”
- Keep it visible – Put those running shoes in a high visibility area of your home so that you have a visual reminder to gear up and get outside for a jog. Are you using a theraband for your exercise routine? Don’t hide it – hang it in plain sight so that you are prompted to put it to good use!
- Teach what you’ve learned – If you have mastered a new exercise or healthy recipe, share it! Pay it forward and reap the benefit of better understanding through teaching. You know you have truly mastered a technique when you can teach it effectively to someone else.
So let me know – what do you do to encourage yourself to follow through with your commitments to yourself? Have you tried any of these suggestions before? Do you have new ideas you’d like to share with us? Let’s support each other in making 2018 a year of abundant good health!
More
What do a toy poodle and the human head have in common? They both share an average weight of 10-12 pounds. Your spine has three natural shock-absorbing curves which attenuate the stress of bearing that load above your shoulders while you move through your day. With good posture and frequent position changes, most of us can bear that weight without difficulty.
However, the moment you drop your chin to read the latest blog update on your cell phone the balance changes completely. When your head inclines forward 60 degrees the force your neck is bearing is equivalent to exchanging that toy poodle for a Labrador retriever – 60 pounds of force (Hansraj, 2014)! Consider that the average person sustains this position for 2-4 hours a day while using their smart phone and the load quickly becomes overwhelming. This chronic fatigue to the muscles and structure of the neck can lead to debilitating injury.
Your neck will thank you for contacting Nick Rinard Physical Therapy to address your posture.
Let us help you get that heavy Labrador off your shoulders!
Hansraj, KK. “Assessment of stresses in the cervical spine caused by posture and position of the head.” Surgical Technology International. 2014, November; 25:277-9
More
At Nick Rinard Physical Therapy a lot of patients come to see us with knee pain and/or knee arthritis, both before and after various knee surgeries, including total knee replacement surgeries.
Since 2010, knee replacements have been the most performed surgery on people over 45 years of age. Knee replacements are performed at the rate of 700,000 per year. Because of this increasing rate, the efficacy of pain relief and improvement of function should be investigated.
100 patients with knee arthritis
A researcher, Soren Thorgaard Skou, has done just that. In his study, he looked at 100 patients with knee arthritis and assigned them to a surgical group or non-surgical group (which received physical therapy, medication and diet education). After one year, 85% percent of the surgical group had significant improvements in pain vs 68% of the physical therapy group. The surgical group and larger gains in their ability to climb stairs and walk. However, the study also showed that the surgical group is at greater risk for complications that the physical therapy group is not. The surgical group is more likely to have blood clots or a manipulation (another procedure performed by the surgeon to increase range of motion). The surgical group had more adverse side effects vs the physical therapy group (24 vs. 6).
Physical therapy is effective
Physical therapy is effective and should be considered a viable option before jumping to surgery. If the first knee replacement can be delayed, this can decrease the necessity for a second surgery (current replacements last 10-15 years). We urge our patients to remember that we are always here for you before or after surgery. Nick Rinard Physical Therapy is a phone call away 503-244-6232 !
1/3rd of knee replacements are unnecessary
This, taken into consideration with the study that came out last summer that found nearly 1/3rd of knee replacements are unnecessary, should be considered when deciding to have a knee replacement or a trial of physical therapy to determine effectiveness.
Sources:
http://health.usnews.com/health-news/articles/2015/10/21/knee-replacement-brings-less-pain-better-function
Dr. Skou’s report (N Engl J Med. 2015 373;17:1668-9)
More
Many times we have patients who come for physical therapy treatment describing pain in their leg, but it turns out to be coming from their spine. This is often confusing for people, especially if they have been given a provisional medical diagnosis related to the area of pain, like “piriformis syndrome”, which is pain in one of your gluteal muscles. You may wonder how we determine where the pain is coming from and what to treat. Pain is produced by sensory nerves. Sensory nerves can be triggered locally at the spinally level, or peripherally either by muscle tension or injury. During the evaluation we always perform spine ROM to determine if the source could be coming from the spine. The screen must begin from the center outward. In some cases, knee/hip/ankle pain will decrease or increase during the lumbar spine screen, and then we know it is coming from the spine. This can be hard to understand for some patients because the pain they are experiencing feels like it is coming from that very spot, whether it is a joint or muscle, that is painful. For example, I recently evaluated a patient with ankle pain. She had even fallen, which made it possible she could have some trauma to her ankle from the fall. However, during the lumbar spine screen, her ankle pain decreased while performing a back bend. She was in disbelief that her ankle pain went away. After only a few visits her ankle pain was gone and it did not return. One of her lumbar discs was pressing on a nerve root and causing her ankle pain, and the back bending pushed the disc away from the nerve and abolished the pain. The moral of the story is, we can never assume a diagnosis until a thorough examination is performed.
More
By Nick Rinard MPT, Cert MDT
20 Apr, 2017
Physical Therapy Tips
bone, Cert. MDT, false positive, findings, imaging, joint, MRI, Nick Rinard MSPT, roles, x-ray
 “Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
“Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
First, physical therapists can make an accurate clinical diagnosis that will most likely match the radiological diagnosis. A 2005 study published in the Journal of Orthopedic and Sports Physical Therapy compared the agreement between what the physical therapist thought the imaging would show, and what doctors thought the imaging would show. “Clinical Diagnostic Accuracy and Magnetic Resonance Imaging of Patients Referred by Physical Therapists, Orthopedic Surgeons, and Non-orthopedic providers.” Physical therapists could predict the correct imaging diagnosis 74.5% of the time! That’s almost as accurate as orthopedic surgeons, and over twice as good as general practitioners!
- Physical Therapists = 74.5% (108/145)
- Orthopedic Surgeons = 80.8% (139/172)
- Non-orthopedic = 35.4% (86/243)
So, only in a small number of cases, will you need an x-ray or MRI to help determine your condition if it cannot be determined clinically.
False positives
Second, there are a lot of “false positive” findings associated with imaging. A false positive is when the test (radiologic image) shows you have the disease or condition, when you actually don’t. Some of you readers may know of people who were freaked out by a “finding” on their mammogram that turned out (luckily) to not be cancer. How often does this happen in the joints or spine that a physical therapist treats? If you are talking about the neck, quite a lot of people with NO NECK PAIN have a “major finding” on MRI. It is broken down below. (From The Journal of Bone and Joint Surgery 1990 “Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation”)
For people less than 40 years old:
- Major abnormality in 14%
- Herniated disc = 10% (of subjects)
- Foraminal stenosis = 4%
- No “major” bulging discs were seen
- Narrowed disc space / degenerated discs = 25%
- Cord abnormalities = 9%
For people older than 40 years:
- Major abnormality in 28%
- Herniated disc = 5%
- Foraminal stenosis = 20%
- Only 1 subject “major” bulging disc was seen
- Narrowed disc space / degenerated discs = 57%
- Cord abnormalities = 1%
Remember, these are findings in people with NO NECK PAIN. If you have neck pain, there is a good chance that you might have one of these findings, but it would not be the source of your pain. The study authors conclude: “The prevalence of cervical spine pathology in asymptomatic (pain free) individuals of a wide-range of ages, points out the danger in ordering surgery or invasive procedures, or even giving the patient an ominous-sounding diagnosis, without first correlating these MRI findings with clinical signs and symptoms.”
Imaging the lumbar spine can also lead to errors as there is even greater incidence of false positive MRI findings in asymptomatic subjects in the lower back as compared to the neck…
“Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation.” J Bone Joint Surg Am. 1990
- 33% had a “substantial” abnormality
60 years old:
- 36% had a disc herniation
- 21% had spinal stenosis
Accurate Diagnosis with your Physical Therapist
If you are still reading this article, then you must be interested in getting an accurate diagnosis of your problem, and you might think a physical therapist could be the one person who can do that. You would be right. Plus, a physical therapist will offer you treatment for your condition, not surgery or drugs. I have been convinced beyond a doubt in my 20 plus years of practice that one should start with a good physical therapy evaluation and possibly treatment before turning to x-ray or MRI. A good physical therapist knows when the clinical diagnosis is complete and correct and when imaging is needed to help fill in the blanks. Don’t get an x-ray or MRI first. It might point you in the wrong direction and bias the clinician trying to arrive at the correct diagnosis and treatment. If you truly need imaging, your physical therapist at Nick Rinard Physical Therapy can help guide you in that decision.
More
 The American Heart Association recommends at least 30 minutes of moderate-intensity aerobic activity at least 5 days/week. In the pursuit of good health and fitness, many people are using YouTube to access new workouts. Unfortunately, there is neither quality control nor an accreditation process to ensure that the workouts are sound. Further complicating things is the “no pain, no gain” exercise myth which leads people to expect suffering with exercise. If someone expects exercising to be painful, they may not heed the early warning signs of pain and become injured.
The American Heart Association recommends at least 30 minutes of moderate-intensity aerobic activity at least 5 days/week. In the pursuit of good health and fitness, many people are using YouTube to access new workouts. Unfortunately, there is neither quality control nor an accreditation process to ensure that the workouts are sound. Further complicating things is the “no pain, no gain” exercise myth which leads people to expect suffering with exercise. If someone expects exercising to be painful, they may not heed the early warning signs of pain and become injured.
Recently, I treated a young woman who developed severe lower back pain after exercising with a popular fitness program online. She continued to push herself through the routines but after 2 weeks she quit exercising entirely. She was frustrated because her efforts to improve her health had actually worsened her condition. Her back pain was interrupting her sleep and limiting her ability to concentrate at work.
After just 4 sessions at Nick Rinard Physical Therapy she was pain free and equipped with an effective, individualized exercise program that supported her fitness goals without compromising her If your workout is wearing you down, we can help you get on the right track! Don’t settle for suffering through your exercise routine when you could be thriving.
More
By Margo Burette, DPT
08 Aug, 2016
Posture
assessment, cervical spine, chin, common, contact, posture, power, stresses, Toy poodle

What do a toy poodle and the human head have in common? They both share an average weight of 10-12 pounds. Your spine has three natural shock-absorbing curves which attenuate the stress of bearing that load above your shoulders while you move through your day. With good posture and frequent position changes, most of us can bear that weight without difficulty.
However, the moment you drop your chin to read the latest blog update on your cell phone the balance changes completely. When your head inclines forward 60 degrees the force your neck is bearing is equivalent to exchanging that toy poodle for a Labrador retriever – 60 pounds of force (Hansraj, 2014)! Consider that the average person sustains this position for 2-4 hours a day while using their smart phone and the load quickly becomes overwhelming. This chronic fatigue to the muscles and structure of the neck can lead to debilitating injury.
Your neck will thank you for contacting Nick Rinard Physical Therapy to address your posture.
Let us help you get that heavy Labrador off your shoulders!
Hansraj, KK. “Assessment of stresses in the cervical spine caused by posture and position of the head.” Surgical Technology International. 2014, November; 25:277-9
More
This is a placeholder for the Newsletter plugin images. You may edit and reuse this post but do not remove it.
More



 “Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
“Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first. The American Heart Association recommends at least 30 minutes of moderate-intensity aerobic activity at least 5 days/week. In the pursuit of good health and fitness, many people are using YouTube to access new workouts. Unfortunately, there is neither quality control nor an accreditation process to ensure that the workouts are sound. Further complicating things is the “no pain, no gain” exercise myth which leads people to expect suffering with exercise. If someone expects exercising to be painful, they may not heed the early warning signs of pain and become injured.
The American Heart Association recommends at least 30 minutes of moderate-intensity aerobic activity at least 5 days/week. In the pursuit of good health and fitness, many people are using YouTube to access new workouts. Unfortunately, there is neither quality control nor an accreditation process to ensure that the workouts are sound. Further complicating things is the “no pain, no gain” exercise myth which leads people to expect suffering with exercise. If someone expects exercising to be painful, they may not heed the early warning signs of pain and become injured.