By Nick Rinard MPT, Cert MDT
20 Apr, 2017
Physical Therapy Tips
bone, Cert. MDT, false positive, findings, imaging, joint, MRI, Nick Rinard MSPT, roles, x-ray
 “Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
“Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
First, physical therapists can make an accurate clinical diagnosis that will most likely match the radiological diagnosis. A 2005 study published in the Journal of Orthopedic and Sports Physical Therapy compared the agreement between what the physical therapist thought the imaging would show, and what doctors thought the imaging would show. “Clinical Diagnostic Accuracy and Magnetic Resonance Imaging of Patients Referred by Physical Therapists, Orthopedic Surgeons, and Non-orthopedic providers.” Physical therapists could predict the correct imaging diagnosis 74.5% of the time! That’s almost as accurate as orthopedic surgeons, and over twice as good as general practitioners!
- Physical Therapists = 74.5% (108/145)
- Orthopedic Surgeons = 80.8% (139/172)
- Non-orthopedic = 35.4% (86/243)
So, only in a small number of cases, will you need an x-ray or MRI to help determine your condition if it cannot be determined clinically.
False positives
Second, there are a lot of “false positive” findings associated with imaging. A false positive is when the test (radiologic image) shows you have the disease or condition, when you actually don’t. Some of you readers may know of people who were freaked out by a “finding” on their mammogram that turned out (luckily) to not be cancer. How often does this happen in the joints or spine that a physical therapist treats? If you are talking about the neck, quite a lot of people with NO NECK PAIN have a “major finding” on MRI. It is broken down below. (From The Journal of Bone and Joint Surgery 1990 “Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation”)
For people less than 40 years old:
- Major abnormality in 14%
- Herniated disc = 10% (of subjects)
- Foraminal stenosis = 4%
- No “major” bulging discs were seen
- Narrowed disc space / degenerated discs = 25%
- Cord abnormalities = 9%
For people older than 40 years:
- Major abnormality in 28%
- Herniated disc = 5%
- Foraminal stenosis = 20%
- Only 1 subject “major” bulging disc was seen
- Narrowed disc space / degenerated discs = 57%
- Cord abnormalities = 1%
Remember, these are findings in people with NO NECK PAIN. If you have neck pain, there is a good chance that you might have one of these findings, but it would not be the source of your pain. The study authors conclude: “The prevalence of cervical spine pathology in asymptomatic (pain free) individuals of a wide-range of ages, points out the danger in ordering surgery or invasive procedures, or even giving the patient an ominous-sounding diagnosis, without first correlating these MRI findings with clinical signs and symptoms.”
Imaging the lumbar spine can also lead to errors as there is even greater incidence of false positive MRI findings in asymptomatic subjects in the lower back as compared to the neck…
“Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation.” J Bone Joint Surg Am. 1990
- 33% had a “substantial” abnormality
60 years old:
- 36% had a disc herniation
- 21% had spinal stenosis
Accurate Diagnosis with your Physical Therapist
If you are still reading this article, then you must be interested in getting an accurate diagnosis of your problem, and you might think a physical therapist could be the one person who can do that. You would be right. Plus, a physical therapist will offer you treatment for your condition, not surgery or drugs. I have been convinced beyond a doubt in my 20 plus years of practice that one should start with a good physical therapy evaluation and possibly treatment before turning to x-ray or MRI. A good physical therapist knows when the clinical diagnosis is complete and correct and when imaging is needed to help fill in the blanks. Don’t get an x-ray or MRI first. It might point you in the wrong direction and bias the clinician trying to arrive at the correct diagnosis and treatment. If you truly need imaging, your physical therapist at Nick Rinard Physical Therapy can help guide you in that decision.
More
By Nick Rinard MPT, Cert MDT
09 Jun, 2014
Clinical Case of the Week
abduction, chronic, dosed loading, dysfunction, falling, flexion, remodeling, shoulder pain, suprapinatus
 Patient is a 60 y/o male “Mike” with chronic shoulder pain. Mike’s symptoms started in 1994 after falling onto his left shoulder. Overall, his symptoms had been unchanging and severely affecting his job. He has had previous physical therapy and massage therapy to no avail. He was severely limited with lifting, carrying and working out.
Patient is a 60 y/o male “Mike” with chronic shoulder pain. Mike’s symptoms started in 1994 after falling onto his left shoulder. Overall, his symptoms had been unchanging and severely affecting his job. He has had previous physical therapy and massage therapy to no avail. He was severely limited with lifting, carrying and working out.
During his initial evaluation, it was found that Mike had painful, limited range of all shoulder movements with the exception of lateral rotation. He also had weak/painful resisted tests of shoulder abduction, medial rotation and flexion. His most limited impairment was painful, weak abduction.
It was determined that Mike had chronic dysfunction of the supraspinatus muscle tendon (one of the rotator cuff muscles). Because of the anatomical position of this tendon, it is the most commonly injured and torn of the rotator cuff. Mike began remodeling his tendon with targeted, dosed loading. By the next visit, he was strong, in less pain and had improved range of motion.
Mike continued his remodeling exercises for the next 4 weeks. By his 6th visit to our Portland clinic he had virtually no pain and was no longer limited with his work or life from his shoulder pain. Mike is a classic example of how conservative treatment that targets the root of the problem results in fast, effective results!
Don’t wait 20 years to have your simple problem solved. Have a mechanical evaluation at Nick Rinard Physical Therapy today!
More
By Nick Rinard MPT, Cert MDT
07 Mar, 2014
Clinical Case of the Week, Exercise, Physical Therapy Tips
abolished, cervical, MDT, neck pain, shoulder, sugery, true cause of pain
 Very interesting clinical presentation today! The patient had been treated for neck pain here (Nick Rinard Physical Therapy) in the past with good results. Later, she developed shoulder pain and consulted her MD, who referred her to an orthopedic surgeon. There were “findings” on MRI and she ended up getting arthroscopic surgery. She returned to us for physical therapy to rehabilitate after surgery.
Very interesting clinical presentation today! The patient had been treated for neck pain here (Nick Rinard Physical Therapy) in the past with good results. Later, she developed shoulder pain and consulted her MD, who referred her to an orthopedic surgeon. There were “findings” on MRI and she ended up getting arthroscopic surgery. She returned to us for physical therapy to rehabilitate after surgery.
No Surgery Needed
Interestingly, she reported that her surgeon was surprised that her rotator cuff tendons were in “good condition” and did not require a repair – he had noticed that during the surgery procedure itself, apparently. So, physical therapy should be easy in such cases, right? No big surgical repair to worry about.
However, 6 weeks after the operation, her shoulder pain was not subsiding as it should have. Inflammation normally resolves in that amount of time and she should have been strong enough to resume normal office work duties consisting of keyboard and filing.
Finding the True Cause of the Pain
We had to take a closer look at her neck. It turned out that her neck was referring pain to the shoulder! In one neck treatment, the shoulder pain was abolished! The patient probably had had a recurrence of her old neck problem, it referred pain to her shoulder, and neither she, her MD, nor the orthopedic surgeon considered the true cause of the pain…
This is a frequent occurrence here at Nick Rinard Physical Therapy, where we use the Mechanical Diagnosis and Therapy (MDT) system of evaluation and treatment. Robin McKenzie started this method and it is the best method – and most supported by research – at getting to the true cause of pain.
Save time, money, and maybe avoid surgery!
If you or someone you know is having any problems that could be mechanical, a thorough mechanical assessment should be performed. In as little as one visit the problem might be identified and solved, saving a lot of time, money, and suffering! Plus, the patient might avoid unnecessary surgery!
More
LOW BACK PAIN—What you should do while waiting for your first physical therapy appointment…
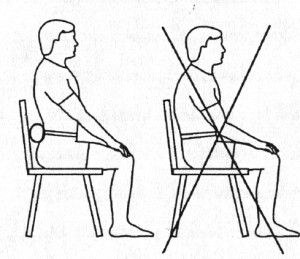
SITTING:
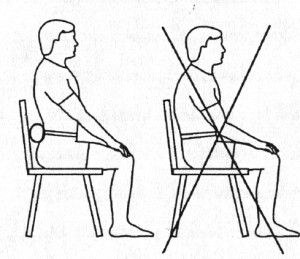 Sit as little as possible. Standing or lying down are preferable to sitting when in acute low back pain. If you must sit, sit only in a straight backed chair with good posture. Avoid couches or soft chairs. Use a towel roll to support the natural curve of your spine.
Sit as little as possible. Standing or lying down are preferable to sitting when in acute low back pain. If you must sit, sit only in a straight backed chair with good posture. Avoid couches or soft chairs. Use a towel roll to support the natural curve of your spine.
BENDING:
Do not bend forwards as in touching your toes when in acute low back pain—even if it feels like you are doing good by “stretching” the muscles of the low back. Rather than reaching down to get things, squat down using the legs and keep the back absolutely straight.
LYING:
Try to lie more on your stomach rather than on your back. Avoid the temptation to lie on your back with the head and knees propped up—this just rounds the back more and places inappropriate stress on injured structures.

EXERCISES:
You should stay normally active–in other words try not to stay in bed for long periods. Move around, take walk if you can. Do not do the knees to chest exercise you may have learned before. This is an advanced exercise and usually not appropriate for acute conditions. It is better in most cases to lie on your stomach and work towards supporting yourself on the elbows.
 |
 |
| NO! |
YES! |
More
 The case study I would like to share with you today is only the second hip derangement of this type that I have seen in 18 years of practice. “Jim” was a 55 year old male who presented with right hip pain that started for no apparent reason 5-6 months prior to coming to physical therapy. He said the pain was provoked only when he was walking, but it occurred consistently at a distance of about 50 to 100 yards. Often it was so painful he could not continue walking. Jim figured out that changing his right foot position enabled him to walk a little further, albeit slowly, and then he could resume normal walking for another 50 yards or so. He would change the foot position by stepping partway onto a curb or raised ground such that the outer edge of his foot was tilted up (eversion, as we therapists call it), and then he would angle his right knee inwardly. That was the only way he had found to improve walking, but the hip just would not stay better.
The case study I would like to share with you today is only the second hip derangement of this type that I have seen in 18 years of practice. “Jim” was a 55 year old male who presented with right hip pain that started for no apparent reason 5-6 months prior to coming to physical therapy. He said the pain was provoked only when he was walking, but it occurred consistently at a distance of about 50 to 100 yards. Often it was so painful he could not continue walking. Jim figured out that changing his right foot position enabled him to walk a little further, albeit slowly, and then he could resume normal walking for another 50 yards or so. He would change the foot position by stepping partway onto a curb or raised ground such that the outer edge of his foot was tilted up (eversion, as we therapists call it), and then he would angle his right knee inwardly. That was the only way he had found to improve walking, but the hip just would not stay better.
In desperation, Jim said he had looked online and tried numerous “hip exercises” without any relief. He consulted his doctor, who recommended MDT, which we do here at Nick Rinard Physical Therapy.
Assessment
The mechanical assessment was positive for only two findings: limited and painful hip motion into flexion (folding the knee to chest), and weak and painful testing of hamstring resistance. The protocol for ruling out a joint derangement is to repeat motions to determine if the baselines change. The question is which motion to repeat. One can move either into the most painful direction, go the opposite direction, or check rotations. I chose to go into the most painful direction, in this case, flexion. But before testing I wanted to establish how far Jim could walk in the clinic before his pain started. By the time he walked one length of the hallway and back, he reported pain. I then instructed Jim to bend his knee to chest (compressing the groin) repeatedly and after 20 to 30 times. It produced his familiar pain initially, then the pain abolished and his motion increased. I tested walking after that and Jim said there was no pain even after walking 3 lengths up and back through the hallway! I gave Jim his exercises and scheduled him for 2 days later.
Progress
When Jim returned he reported that he could walk longer distances without the pain starting, however, he still got to the point where he had to modify his foot position in order to continue. I knew we were on the right track, and the next step in treating a joint derangement is to progress forces. I did this manually by applying over-pressure, and instructed Jim to do it in standing by folding his chest down to his knee with it supported on a bench or chair. By the next visit, Jim reported that this had worked very well and he had not experienced any pain at all! So, the derangement was reduced and I needed to wean him off the home exercises to see if it would return or not. I gave him the weaning program and asked to see him back in 2 weeks.
Pain Free
After 2 weeks, Jim came back reporting that he had been able to walk unlimited distances! He resumed walking his dog, going on walks for exercise, and walking wherever, and whenever he wanted. He reported his longest walk lasted 4.5 hours. He said there was no return of the original hip pain from which he had suffered for months. However, on his last two walks, he had started noticing a new hip pain, this time in the front, not on the sides. I re-checked his baselines and neither flexion motion nor resisted hamstrings were painful. That meant it could not be a re-derangement. Resisted hip flexion was painful, and that was new. I concluded that his sudden ability to walk pain-free resulted in his over-doing it. Jim had increased walking too fast and gotten a minor tendonitis. That was easy to treat, and by his next visit, Jim was pain-free again and able to progress walking, though this time more gradually, which was safer.
Successful Treatment
Jim’s hip treatment was obviously a success. It took only 4 visits. This hip derangement was unique because the direction that reduced it (flexion); I have only seen one other hip derangement require flexion to reduce it. The fact that Jim resumed normal activity too fast is typical of reduced derangements – the patient feels so good that they over do it. Luckily in Jim’s case, we found the new problem and fixed it just as fast as we found and fixed his chronic hip pain.
More
TMJ pain can be a real problem for its victims, limiting their ability to chew and talk, and interrupting sleep. Often, headaches even limit the person’s ability to concentrate! Various treatments have been proposed to alleviate the symptoms of TMJ (Temporomandibular Joint) pain, many of which are very complex and even invasive. Looking at the TMJ as “just another joint” and not predetermining that it has to be complicated has been very freeing for me in using a mechanical approach. Let me explain using a patient example from this week in clinic.
My approach is modeled after the McKenzie Method of Mechanical Diagnosis and Therapy, although very little about TMJ specifically has been written or published about it. (1)
Symptoms and Experience
Now, about the patient. (Name and other identifying information has been omitted to protect privacy). This patient complained of intermittent left jaw pain with wide opening of the mouth. He stated it only occurred then, and otherwise it really was not painful. However, chewing tough foods, he admitted, was sometimes painful. His worst pain occurred with rapid opening of the mouth and could be as intense as 6 on a scale of 1-10.
Therapist’s Evaluation and Findings
Objective findings were limited and painful opening with slight left deviation, limited and painful protrusion, limited and painful right deviation, and no pain or limitation with retraction, or left deviation. Repeated tests performed actively by the patient of protrusion first, then of right deviation resulted in producing the patient’s symptoms, no worse after, but also no change in baseline ROM or pain. Forces were progressed to patient applied over-pressure to right deviation. The patient reported that this produced his pain initially, then decreased pain as he performed more repetitions. Subsequently, he reported wider opening with less pain!
Patient Homework
Home exercises were assigned, which naturally consisted of patient applied over-pressure into repeated right deviation every hour or two as per typical McKenzie protocol. On the second clinic visit two days later, the patient stated he was already 50% improved! This finding confirmed the mechanical diagnosis of derangement syndrome. In this classification, there is a good prognosis for rapid and lasting recovery from the problem.
Get Yourself Evaluated
This is only one clinical example of a purely mechanical TMJ problem. While there are examples of TMJ issues that are not derangements, or even mechanical, often a mechanical cause of the pain can be found and the patient helped by mechanical therapy. It is well worth a thorough examination to determine if your TMJ pain has a mechanical component, and to get appropriate treatment which would otherwise be missed.
(1) http://www.sciencedirect.com/science/article/pii/S1356689X1100230X
More
This week I will tell you about the rapid recovery of an ipsilateral shift. An ipsilateral shift was described by Robin McKenzie of the McKenzie Method®, and the treatment of this patient of the week follows Mechanical Diagnosis and Therapy® principles exactly as I was taught them. The patient presents with a lateral shift deformity of the trunk shifted away from the side of dominant pain.
Gerry, (not his real name), arrived with his wife to clinic after suffering 10/10 pain in his back, buttock, and thigh, and had a severe ipsilateral shift. This had been present for 2 weeks, and Gerry stated it had recently worsened after a massage session. Gerry could not recall any incident that caused injury or otherwise caused the onset of pain. He stated he had tried standard chiropractic treatment with no effect.
While I was taking Gerry’s history, his wife reported that he had to crawl to get around their home for the first hour after getting out of bed. Even at his best, he could barely make it down the hall to my office. He was completely unable to dress himself, drive or go to work.
The shift made the mechanical diagnosis easy. It was most likely a mechanical derangement. Any attempt Garry made to bend forward or backward resulted in severe pain, and nearly no range of motion. Trying to correct the shift himself, even when leaning against the wall for support, also resulted in severe pain and no gain in range of motion.
Therefore, manual forces had to be applied by the MDT therapist – in this case – me! (I have achieved certification in Mechanical Diagnosis and Therapy® by the McKenzie® Institute, designated by “Cert. MDT”).
Manual shift correction is described in various published works by Robin Anthony McKenzie, the originator of the McKenzie® Method of Mechanical Diagnosis and Therapy®. It involves full body pressure against the hips and opposite side of the trunk provided by the therapist. It can be painful to experience, however, only pain that centralizes is permitted, according to McKenzie®. As I learned in my McKenzie® training from expert therapist Colin Davies, the duration of force application can last a long time – up to 45 minutes. Gerry’s shift was challenging. I applied force for 45 minutes, but still there was only minimal correction of his shift!
By day two, Gerry could walk better, but was still shifted. This time, manual force corrected the shift in 15 minutes. The next day Gerry could correct his own shift and he was not taking any pain medication anymore!
Now, one week later, he is no longer shifted at all. He can dress himself, including his socks and shoes, drive, and go to work. Regarding walking, he only needed to swing his Right arm normally again – he had been supporting his back with it and lost normal gait in the interim. He reported pain levels of 1-2/10.
Treating Gerry was very satisfying. His mechanical diagnosis was clear, treatment was difficult, but not confusing. I credit the McKenzie® Method of Mechanical Diagnosis and Therapy® with giving me the expertise to be so successful in treating this, and other painful spine and joint conditions. Thank you for your interest in the clinical case study of the week!
Nick Rinard MPT, Cert MDT
More
This is about a shoulder derangement that was identified, and fixed in 10 minutes. But there is more background to the story.
Debbie (a fictitious name for the real person) was training for her first 1/2 Marathon, held in Portland, Oregon. About 3 weeks before the event she presented to physical therapy complaining of pain behind the knee. Such an injury so close to a sporting event is automatically worrisome because it threatens participation. Both Debbie and I were concerned that it could stop her from being able to run the 1/2 marathon!
I performed a mechanical assessment per the McKenzie Method, combined with Cyriax style selective tissue tension tests, and diagnosed the knee pain as “semitendinosis tendinitis”, named according to Laslett nomenclature. It is a lesion of the hamstring.
Although Debbie had good hamstring flexibility, I deduced, based on her history (she was certified as a yoga instructor), that she normally had more. Treatment consisted of stretching out her hamstrings, combined with manual deep tissue mobilization of the hamstring muscle belly. It worked!
She ran the 1/2 Marathon without any knee pain! However, her shoulder became painful during the event! She asked me to look at it 4 days later since it had not subsided on its own.
She presented with what appeared to be a clear contractile lesion of the infraspinatus tendon, with a weak resisted test of lateral rotation. However, there were two pieces of information that were inconsistent with this conclusion. 1) Resisted shoulder flexion was painful with the elbow positioned behind the body, but painless with the elbow in front. 2)
There was no tenderness at all near the infraspinatus tendon, which would be typical , but not required, for the lesion to be harbored in the infraspinatus tendon.
Further mechanical assessment was needed, and this followed the McKenzie Method of Mechanical Diagnosis and Therapy. Repeated tests would differentiate between a derangement and other possible pathologies. I surmised that the arm bone could have been malpositioned in the shoulder girdle from Debbie pumping her arms while running. The logical step was to reverse the activity of arm pumping and correct the derangement. So I instructed her to reach all the way across her body with that arm and then push it further using the other hand. This became less and less painful until there was no pain! Furthermore, it resulted in much less pain produced by resisted flexion afterward! Another exercise–that of rotating the arm bone back into place–worked well also, virtually rendering all prior painful tests, painless!
Needless to say, Debbie was very pleased with both the rapid results with her shoulder, and grateful that her knee pain was treated in time for her to complete her 1/2 marathon!
More
Medical Advisory: MDT is a Superior Form of Physical Therapy
This is page 2, continued from <<Choose your Physical Therapist Wisely
If you sustained your injuries in a motor vehicle accident, or work-related injury, then your chances of getting better are improved if you choose an MDT therapist. There is a financial advantage also since the total cost of your therapy will be less, based on the fewer number of visits MDT uses. Your PIP money will go further, and you will not have to sacrifice a large amount of money out of your settlement just to pay high physical therapy bills. If you are a worker, your case will be less likely to be denied if you are getting better faster, than if your recovery drags on. Believe me, insurance adjusters are less likely to keep your case open if you are not improving in physical therapy.
So you can see that MDT is a superior form of physical therapy. What about MDT compared to Chiropractic care? I tell my patients that Chiropractic treatment is indeed mechanical, but there are two distinct reasons it is not superior to MDT. The first reason has to do with the evaluation, and the second reason has to do with the treatment. A chiropractor first must take an X-ray to make the diagnosis. Unfortunately, there is little evidence to suggest a chiropractic diagnosis is reliable, and therefore, treatment based on an unreliable diagnosis is a guess at best. Secondly, chiropractic treatment is performed to the patient, not by the patient. Any improvement in the patient’s condition, therefore, is dependent on them going back for more visits! As mentioned, MDT treatments consist primarily of exercises that the patient performs so you can treat yourself when not in the clinic. This obviously results in less pain, a speedier recovery, less visits, and money saved!
By reading this essay, you are now equipped with knowledge to seek out the best care possible for your injuries. Don’t waste time going to traditional physical therapy, or chiropractic for many visits. It is better to get an MDT evaluation to determine if your condition will respond mechanically or not, and if it is mechanical, then the treatment is more effective and takes less time!
In closing, I would like to mention how MDT compared to traditional physical therapy in an objective study conducted by a third party. The average improvement in traditional physical was only 78 percent, and it took an average of 11 visits to achieve this. By contrast, MDT got patients 93 percent better in only 6.5 visits! The data speak for themselves. Don’t settle for less effective treatment for your injury – find a Cert MDT therapist who is using the MDT method properly, and get better faster!
Nick Rinard is president of, and a therapist at, Nick Rinard Physical Therapy, a private physical therapy clinic.
More
Medical Advisory: Choose Your Physical Therapist Wisely
by
The purpose of this essay is to inform you that not all Physical Therapy is the same. Some are more effective than others. If you had Physical Therapy, did it work? If you are going to Physical Therapy now, is it helping? If yes, you should continue until you are better. However, if you are not getting better, or if you need Physical Therapy in the future, then you should read on.
First choice for treating spinal pain
Mechanical Diagnosis and Therapy (MDT) has been shown in numerous scientific studies to be the most effective type of Physical Therapy available today. In a poll of Physical Therapists nationwide, MDT was the first choice for treating spinal pain (APTA publication 2002). This is a good thing, since it shows that the profession of Physical Therapy is gaining more and more scientific evidence to support its use. However, you should know just what MDT is so you can be sure you are actually receiving it.
Development of MDT
MDT was developed in New Zealand by a physiotherapist named Robin McKenzie. Mr. McKenzie noticed that his patients got better faster, and could control their pain themselves, compared to patients being treated traditionally. He founded the McKenzie Institute and has been training therapists since 1980. You should choose a therapist that is a certified MDT therapist, designated by Cert MDT.
What – no gadgets?
The MDT method does not rely on technological gadgets such as ultrasound or electrical stimulation commonly used in traditional Physical Therapy. There is little evidence to show that these machines actually help in recovery. Instead, Mechanical Diagnosis and Therapy, as its name suggests, uses mechanical forces to centralize referred pain, and to correct the physical problem. Exercises designed specifically for each patient, affect pain immediately, and can be performed by the patient whenever pain arises. Over a short time, these exercises heal the injury and allow full recovery. In our clinic, Nick Rinard Physical Therapy, the average number of visits is only six and a half!
Your Time is Valuable
A very important part of the MDT method is the evaluation on the first day. A qualified Cert MDT therapist should be able to identify if you will respond or not. This way, if the problem is not mechanical, valuable time in your recovery is not wasted, since you would not go through several weeks of rehabilitation to discover at the end that it did not help. Doctors who have the best interests of their patient in mind prefer MDT for this very reason. If your doctor is not aware of the MDT method, then you can choose an MDT therapist yourself. It is considered standard practice and has been accepted by the medical community.
Medical Advisory: MDT is a Superior Form of Physical Therapy
If you sustained your injuries in a motor vehicle accident, or work-related injury, then your chances of getting better are improved if you choose an MDT therapist. There is a financial advantage also since the total cost of your therapy will be less, based on the fewer number of visits MDT uses. Your PIP money will go further, and you will not have to sacrifice a large amount of money out of your settlement just to pay high physical therapy bills. If you are a worker, your case will be less likely to be denied if you are getting better faster, than if your recovery drags on. Believe me, insurance adjusters are less likely to keep your case open if you are not improving in physical therapy.
MDT compared to Chiropractic
So you can see that MDT is a superior form of physical therapy. What about MDT compared to Chiropractic care? I tell my patients that Chiropractic treatment is indeed mechanical, but there are two distinct reasons it is not superior to MDT. The first reason has to do with the evaluation, and the second reason has to do with the treatment. A chiropractor first must take an X-ray to make the diagnosis. Unfortunately, there is little evidence to suggest a chiropractic diagnosis is reliable, and therefore, treatment based on an unreliable diagnosis is a guess at best. Secondly, chiropractic treatment is performed to the patient, not by the patient. Any improvement in the patient’s condition, therefore, is dependent on them going back for more visits! As mentioned, MDT treatments consist primarily of exercises that the patient performs so you can treat yourself when not in the clinic. This obviously results in less pain, a speedier recovery, less visits, and money saved!
MDT Treatment is more effective and takes less time
By reading this essay, you are now equipped with knowledge to seek out the best care possible for your injuries. Don’t waste time going to traditional physical therapy, or chiropractic for many visits. It is better to get an MDT evaluation to determine if your condition will respond mechanically or not, and if it is mechanical, then the treatment is more effective and takes less time!
Better in only 6.5 visits
In closing, I would like to mention how MDT compared to traditional physical therapy in an objective study conducted by a third party. The average improvement in traditional physical was only 78 percent, and it took an average of 11 visits to achieve this. By contrast, MDT got patients 93 percent better in only 6.5 visits! The data speak for themselves. Don’t settle for less effective treatment for your injury – find a Cert MDT therapist who is using the MDT method properly, and get better faster!
Nick Rinard is president of, and a therapist at, Nick Rinard Physical Therapy, a private physical therapy clinic.
More
 “Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.
“Should I get an x-ray or MRI before physical therapy?” This is a common question, and the answer is – NO. Why not? I hope to clarify that in this article, and give you a convincing reason to try physical therapy first.






 Nick Rinard
Nick Rinard